



 Order Treatment Online
Order Treatment Online
 Diseases and Conditions
Diseases and Conditions

An ankylosing spine in which the vertebrae become fused together.
Ankylosing spondylitis (AS, from Greek ankylos, stiff; spondylos, vertebrae), previously known as Bekhterev's disease, Bekhterev syndrome, and Marie-Strümpell disease, a form of Spondyloarthritis, is a chronic, inflammatory arthritis and autoimmune disease. It mainly affects joints in the spine and the sacroilium in the pelvis, and can cause eventual fusion of the spine.
It is a member of the group of the spondyloarthropathies with a strong genetic predisposition. Complete fusion results in a complete rigidity of the spine, a condition known as bamboo spine.
The typical patient is a young male, aged 20–40, when symptoms of the disease first appear, with chronic pain and stiffness in the lower part of the spine or sometimes the entire spine, often with pain referred to one or other buttock or the back of thigh from the sacroiliac joint.
Men are affected more than women by a ratio about of 3:1, with the disease usually taking a more painful course in men than women. In 40% of cases, ankylosing spondylitis is associated with an inflammation of the eye (iridocyclitis and uveitis), causing redness, eye pain, vision loss, floaters and photophobia. This is thought to be due to the association that these two conditions have with inheritance of HLA-B27. Another common symptom is generalized fatigue and sometimes nausea. Less commonly aortitis, apical lung fibrosis and ectasia of the sacral nerve root sheaths may occur.
When the condition presents before the age of 18, it is relatively likely to cause pain and swelling of large limb joints, particularly the knee. In pre-pubescent cases, pain and swelling may also manifest in the ankles and feet, where calcaneal spurs may also develop.
Pain is often severe at rest, but improves with physical activity. However, many experience inflammation and pain to varying degrees regardless of rest and movement.
Ankylosing spondylitis is one of a cluster of conditions known as seronegative spondyloarthropathies, in which the characteristic pathological lesion is an inflammation of the enthesis (the insertion of tensile connective tissue into bone).

The ankylosis process.
Ankylosing spondylitis (AS) is a systemic rheumatic disease meaning it affects the entire body and is one of the seronegative spondyloarthropathies. Approximately 90% of AS patients express the HLA-B27 genotype, meaning that there is a strong genetic association. However, only 5% of individuals with the HLA-B27 genotype contract the disease. Tumor necrosis factor-alpha (TNF α) and IL-1 are also implicated in ankylosing spondylitis. Autoantibodies specific for AS have not been identified. Anti-neutrophil cytoplasmic antibodies ANCA are associated with AS but don't correlate with disease severity.
The association of AS with HLA-B27 suggests that the condition involves CD8 T cells, which interact with HLA-B. It is not proven that this interaction involves a self antigen and at least in the related Reiter's syndrome (reactive arthritis), which follows infections, the antigens involved are likely to be derived from intracellular microorganisms. There is, however, a possibility that CD4 T cells are involved in an aberrant way, since HLA-B27 appears to have a number of unusual properties, including possibly an ability to interact with T cell receptors in association with CD4 (usually only cytotoxic T lymphocytes with CD8 react with HLAB antigen as it is a MHC class 1 antigen).
There has been a longstanding claim that AS arises from a cross-reaction between HLA-B27 and antigens of the Klebsiella bacterial strain (Tiwana et al. 2001). The problem with this idea is that no such cross reactivity with B27 has been found (i.e. although antibody responses to Klebsiella may be increased, there is no antibody response to B27, so there seems to be no cross reactivity.) Particular authorities argue that elimination of the prime nutrients of Klebsiella (starches) would decrease antigenemia and improve the musculoskeletal symptoms. However, as Khan (2002) argues, evidence for a correlation between Klebsiella and AS is circumstantial so far, and that the efficacy of low-starch diets has not yet been scientifically evaluated. Studies on low-starch diet and AS could be difficult to fund, while new biologics developed by the pharmaceutical industry may demonstrate efficacy, as well as financial benefit to the industry (whereas changing the diet would not).
Toivanen (1999) found no support for the role of Klebsiella in the etiology of primary AS.

Lateral lumbar spine X-ray demonstrating in ankylosing spondylitis.
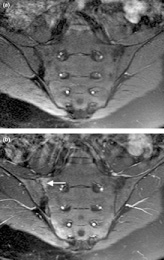
Magnetic resonance images of sacroiliac joints. Shown are T1-weighted semi-coronal magnetic resonance images through the sacroiliac joints (a) before and (b) after intravenous contrast injection. Enhancement is seen at the right sacroiliac joint (arrow, left side of image), indicating active sacroiliitis. This patient had psoriatic arthritis, but similar changes can occur in ankylosing spondylitis.

X-ray showing bamboo spine in a patient with ankylosing spondylitis.
There is no direct test to diagnose AS. A clinical examination and X-ray studies of the spine, which show characteristic spinal changes and sacroiliitis, are the major diagnostic tools. A drawback of X-ray diagnosis is that signs and symptoms of AS have usually been established as long as 8–10 years prior to X-ray-evident changes occurring on a plain film X-ray, which means a delay of as long as 10 years before adequate therapies can be introduced. Options for earlier diagnosis are tomography and magnetic resonance imaging of the sacroiliac joints, but the reliability of these tests is still unclear. The Schober's test is a useful clinical measure of flexion of the lumbar spine performed during examination.
During acute inflammatory periods, AS patients will sometimes show an increase in the blood concentration of C-reactive protein (CRP) and an increase in the erythrocyte sedimentation rate (ESR), but there are many with AS whose CRP and ESR rates do not increase so normal CRP and ESR results do not always correspond with the amount of inflammation a person actually has. Sometimes people with AS have normal level results, yet are experiencing a significant amount of inflammation in their bodies.
Variations of the HLA-B gene increase the risk of developing ankylosing spondylitis, although it is not a diagnostic test. Those with the HLA-B27 variant are at a higher risk than the general population of developing the disorder. HLA-B27, demonstrated in a blood test, can occasionally help with diagnosis but in itself is not diagnostic of AS in a person with back pain. Over 95% of people that have been diagnosed with AS are HLA-B27 positive, although this ratio varies from population to population (only 50% of African American patients with AS possess HLA-B27, and it is close to 80% among AS patients from Mediterranean countries). In early onset disease HLA-B7/B*2705 heterozygotes exhibited the highest risk for disease.
In 2007, a collaborative effort by an international team of researchers in the U.K., Australia and the United States led to the discovery of two genes, ARTS1 and IL23R, that also contribute to the cause of AS. The findings were published in the November 2007 edition of Nature Genetics, a journal that emphasizes research on the genetic basis for common and complex diseases. Together with HLA-B27, these two genes account for roughly 70 percent of the overall incidence of the disease.
The Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), developed in Bath (UK), is an index designed to detect the inflammatory burden of active disease. The BASDAI can help to establish a diagnosis of AS in the presence of other factors such as HLA-B27 positivity, persistent buttock pain which resolves with exercise, and X-ray or MRI evident involvement of the sacroiliac joints. (See: "Diagnostic Tools", below) It can be easily calculated and accurately assesses a patient's need for additional therapy; a patient with a score of 4 out of a possible 10 points while on adequate NSAID therapy is usually considered a good candidate for biologic therapy.
The Bath Ankylosing Spondylitis Functional Index (BASFI) is a functional index which can accurately assess a patient's functional impairment due to the disease as well as improvements following therapy. (See: "Diagnostic Tools", below) The BASFI is not usually used as a diagnostic tool but rather as a tool to establish a patient's current baseline and subsequent response to therapy.
No cure is known for AS, although treatments and medications are available to reduce symptoms and pain.
Physical therapy and exercise, along with medication, are at the heart of therapy for ankylosing spondylitis. Physiotherapy and physical exercises are preceded by medical treatment in order to reduce the inflammation and pain, and are commonly followed by a physician. This way the movements will help in diminishing pain and stiffness, while exercise in an active inflammatory state would just make the pain worse. Normal occupations may be precluded by the symptoms of the disease.
Some may require the help of walking aids such as a cane to help assist in balance and relieve some pressure on affected joints while walking and standing. Many with AS find it very difficult to sit or stand for prolonged periods of time which can even be about 20 minutes, therefore many need to alternate times of sitting and standing, as well as times of rest.
Medical professionals and experts in AS have speculated that maintaining good posture can reduce the likelihood of a fused or curved spine which occurs in a significant percentage of diagnosed persons.
There are three major types of medications used to treat ankylosing spondylitis.
TNFα blockers have been shown to be the most promising treatment, slowing the progress of AS in the majority of clinical cases, helping many patients receive a significant reduction, though not elimination, of their inflammation and pain. They have also been shown to be highly effective in treating not only the arthritis of the joints but also the spinal arthritis associated with AS. A drawback, besides the often high cost, is the fact that these drugs increase the risk of infections. For this reason, the protocol for any of the TNF-α blockers include a test for tuberculosis (like Mantoux or Heaf) before starting treatment. In case of recurrent infections, even recurrent sore throats, the therapy may be suspended because of the involved immunosuppression. Patients taking the TNF medications are advised to limit their exposure to others who are or may be carrying a virus (such as a cold or influenza) or who may have a bacterial or fungal infection.
In severe cases of AS, surgery can be an option in the form of joint replacements, particularly in the knees and hips. Surgical correction is also possible for those with severe flexion deformities (severe downward curvature) of the spine, particularly in the neck, although this procedure is considered very risky.
In addition, AS can have some manifestations which make anaesthesia more complex.
Changes in the upper airway can lead to difficulties in intubating the airway, spinal and epidural anaesthesia may be difficult owing to calcification of ligaments, and a small number have aortic regurgitation. The stiffness of the thoracic ribs results in ventilation being mainly diaphragm-driven, so there may be a decrease in pulmonary function.
All physical therapies must be approved in advance by a rheumatologist, since movements that normally have great benefits to one's health may harm a patient with AS; massages and physical manipulations should only be practiced by therapists familiar with this disease. Some of the therapies that have been shown to benefit AS patients include:
Moderate-to-high impact exercises like jogging are generally not recommended or recommended with restrictions due to the jarring of affected vertebrae that can worsen pain and stiffness in some patients.