

 Order Treatment Online
Order Treatment Online
 Diseases and Conditions
Diseases and Conditions
Rheumatoid arthritis (RA) is a long-term disease that leads to inflammation of the joints and surrounding tissues. It can also affect other organs.
The cause of RA is unknown. It is considered an autoimmune disease. The body's immune system normally fights off foreign substances, like viruses. But in an autoimmune disease, the immune system confuses healthy tissue for foreign substances. As a result, the body attacks itself.
RA can occur at any age. Women are affected more often than men.
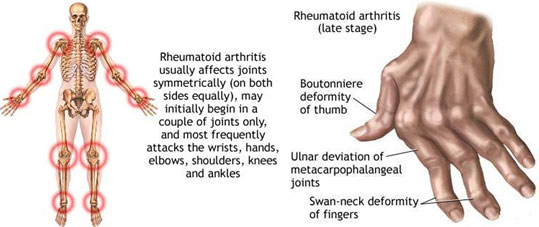
RA usually affects joints on both sides of the body equally. Wrists, fingers, knees, feet, and ankles are the most commonly affected. The course and the severity of the illness can vary considerably. Infection, genes, and hormones may contribute to the disease.
The disease often begins slowly, with symptoms that are seen in many other illnesses:
· Fatigue
· Loss of appetite
· Low fever
· Swollen glands
· Weakness
Eventually, joint pain appears.
· Morning stiffness, which lasts more than 1 hour, is common. Joints can even become warm, tender, and stiff when not used for as little as an hour.
· Joint pain is often felt on both sides of the body.
· The fingers (but not the fingertips), wrists, elbows, shoulders, hips, knees, ankles, toes, jaw, and neck may be affected.
· The joints are often swollen and feel warm and boggy (or spongy) to the touch.
· Over time, joints lose their range of motion and may become deformed.
Other symptoms include:
· Chest pain when taking a breath (pleurisy)
· Eye burning, itching, and discharge
· Nodules under the skin (usually a sign of more severe disease)
· Numbness, tingling, or burning in the hands and feet
Joint destruction may occur within 1 - 2 years after the disease appears.
A specific blood test is available for diagnosing RA and distinguishing it from other types of arthritis. It is called the anti-CCP antibody test. Other tests that may be done include:
· Complete blood count
· C-reactive protein
· Erythrocyte sedimentation rate
· Joint ultrasound or MRI
· Joint x-rays
· Rheumatoid factor test (positive in about 75% of people with symptoms)
· Synovial fluid analysis
Regular blood or urine tests should be done to determine how well medications are working and whether drugs are causing any side effects.
RA usually requires lifelong treatment, including medications, physical therapy, exercise, education, and possibly surgery. Early, aggressive treatment for RA can delay joint destruction.
MEDICATIONS
Disease modifying antirheumatic drugs (DMARDs): These drugs are the current standard of care for RA, in addition to rest, strengthening exercises, and anti-inflammatory drugs.
· Methotrexate (Rheumatrex) is the most commonly used DMARD for rheumatoid arthritis. Leflunomide (Arava) may be substituted for methotrexate.
· These drugs may have serious side effects, so you will need frequent blood tests when taking them.
Anti-inflammatory medications: These include aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen.
· Although NSAIDs work well, long-term use can cause stomach problems, such as ulcers and bleeding, and possible heart problems.
· Celecoxib (Celebrex) is another anti-inflammatory drug, but it is labeled with strong warnings about heart disease and stroke. Talk to your doctor about whether COX-2 inhibitors are right for you.
Antimalarial medications: This group of medicines includes hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine), and is usually used along with methotrexate. It may be weeks or months before you see any benefit from these medications.
Corticosteroids: These medications work very well to reduce joint swelling and inflammation. Because of long-term side effects, corticosteroids should be taken only for a short time and in low doses when possible.
BIOLOGIC AGENTS:
Biologic drugs are designed to affect parts of the immune system that play a role in the disease process of rheumatoid arthritis.
They may be given when other medicines for rheumatoid arthritis have not worked. At times, your doctor will start biologic drugs sooner, along with other rheumatoid arthritis drugs.
Most of them are given either under the skin (subcutaneously) or into a vein (intravenously). There are different types of biologic agents:
· White blood cell modulators include: abatacept (Orencia) and rituximab (Rituxan)
· Tumor necrosis factor (TNF) inhibitors include: adalimumab (Humira), etanercept (Enbrel), infliximab (Remicade), golimumab (Simponi), and certolizumab (Cimzia)
· Interleukin-6 (IL-6) inhibitors: tocilizumab (Actemra)
Biologic agents can be very helpful in treating rheumatoid arthritis. However, people taking these drugs must be watched very closely because of serious risk factors:
· Infections from bacteria, viruses, and fungi
· Leukemia
· Possibly psoriasis
SURGERY
Occasionally, surgery is needed to correct severely affected joints. Surgeries can relieve joint pain and deformities.
The first surgical treatment may be a synovectomy, which is the removal of the joint lining (synovium).
At some point, total joint replacement is needed. In extreme cases, total knee, hip replacement, ankle replacement, shoulder replacement, and others may be done. These surgeries can mean the difference between being totally dependent on others and having an independent life at home.
PHYSICAL THERAPY
Range-of-motion exercises and exercise programs prescribed by a physical therapist can delay the loss of joint function.
Joint protection techniques, heat and cold treatments, and splints or orthotic devices to support and align joints may be very helpful.
Sometimes therapists will use special machines to apply deep heat or electrical stimulation to reduce pain and improve joint mobility.
Occupational therapists can create splints for the hand and wrist, and teach how to best protect and use joints when they are affected by arthritis. They also show people how to better cope with day-to-day tasks at work and at home, despite limitations caused by RA.
Frequent rest periods between activities, as well as 8 to 10 hours of sleep per night, are recommended.
![]()